Ischemic Colitis: When Blood Flow Fails the Colon

- Share via
Key Facts
- Ischemic Colitis occurs when blood flow to part of the colon is reduced or blocked, causing inflammation and potential tissue damage.
- Symptoms can range from mild abdominal discomfort to severe pain and rectal bleeding.
- Risk factors include older age, pre-existing health conditions like heart disease, and physical or surgical stress.
- Diagnosis often involves imaging tests like CT scans, lab work, and endoscopy procedures.
- Treatment varies based on severity, ranging from bowel rest and IV fluids for mild cases to surgery for severe cases with tissue damage.
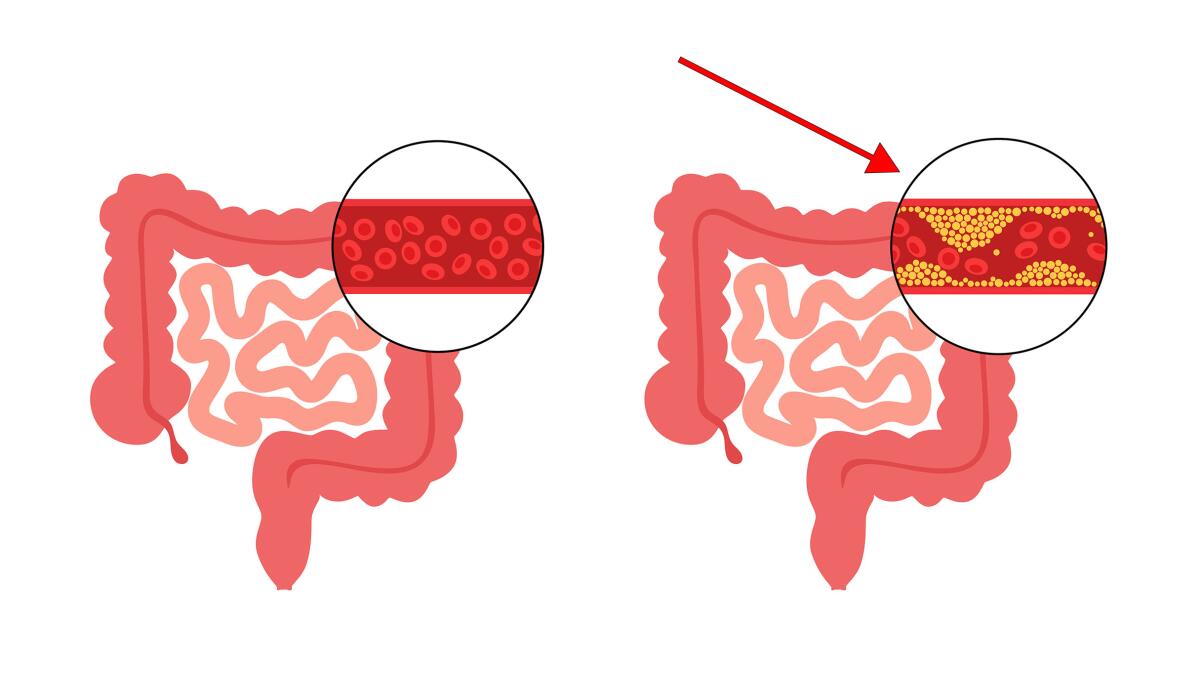
Ischemic colitis (IC) is one of those conditions that doesn’t make headlines but causes big trouble in the gut. It happens when the blood flow to part of the colon slows down or gets blocked temporarily and causes inflammation and in some cases tissue damage.
Although it’s the most common type of ischemic injury to the gastrointestinal tract, IC is underdiagnosed—possibly because the symptoms can be mild or mistaken for something else. Despite this IC accounts for about 1 in 1,000 hospitalizations in the US and the full impact may be bigger than the numbers suggest [4].
Table of Contents
- What causes Ischemic Colitis?
- Ischemic Bowel Disease
- How is Acute Ischemic Colitis Classified?
- What are the Symptoms of Ischemic Colitis?
- What are the Risk Factors?
- Diagnosis of Ischemic Colitis
- How is it treated?
- Surgical Intervention
- Outcome
- Closing Thoughts
- References
What causes Ischemic Colitis?
The causes of ischemic colitis are a combination of different factors working together, usually classified as occlusive (a physical blockage in a blood vessel) or non-occlusive (a temporary drop in blood flow without a blockage) [1], [4]. Surgical procedures such as abdominal aortic aneurysm repair and aortic aneurysm repair can cause ischemic colitis as a rare but serious complication.
Blood clots can cause ischemic colitis by reducing blood flow, so vascular issues are big deal when it comes to gut health.
Here’s how it works:
- Vascular Compromise: The blood vessels feeding the colon—especially the “watershed areas” like the splenic flexure—are prone to reduced blood supply and decreased blood flow.
- Reperfusion Injury: When blood flow returns it paradoxically causes an inflammatory response that can worsen tissue damage [5].
Think of it like pinching a garden hose—when you let go the rush of water can be just as damaging as the pinch itself. That’s what happens in the colon when blood flow is restored too quickly after a period of reduced circulation.
Ischemic Bowel Disease
Ischemic bowel disease, also known as ischemic colitis, is a condition where the blood flow to the large intestine is reduced and the colon wall is inflamed. This can be caused by various factors including low blood pressure, blood clots and constriction of blood vessels.
When ischemic colitis occurs the blood supply to the colon is reduced and tissue dies and can lead to severe complications. Symptoms of ischemic colitis can range from mild to severe and may include abdominal pain, rectal bleeding and bloody diarrhea.
If symptoms persist or worsen over time seek medical attention immediately as early intervention can make a big difference.
How is Acute Ischemic Colitis Classified?
Doctors classify ischemic colitis by how severe it is and how long it lasts:
By Severity:
- Severe IC: Full-thickness (transmural) damage, sometimes leading to multi-organ failure [6]. Acute ischemic colitis can have high morbidity and mortality rates especially when surgery is required.
- Mild IC: Superficial damage, often without systemic complications. Can be managed medically with bowel rest, IV fluids and antibiotics.
By Duration:
- Gangrenous IC: Tissue dies from lack of blood flow (15–20% of cases), can lead to full thickness necrosis.
- Non-gangrenous IC: No tissue death, more common (80–85%) [3], [8].
- Transient or Chronic: Some people recover fully, others deal with long term inflammation and scarring.
What are the Symptoms of Ischemic Colitis?
The classic symptoms are:
- Abdominal pain: Usually sudden, often on the left side. Severe abdominal pain especially with blood in the stool is a critical symptom that requires immediate medical attention.
- Rectal bleeding: Can be obvious (bright red blood) or hidden (occult).
But it’s not always clear cut. In older adults the signs can be subtle—just a general feeling of being unwell or mild discomfort—so it’s easy to miss until it’s serious [2].
Recognizing the signs of ischemic colitis which can appear suddenly or gradually is key to determining the right medical intervention and treatment options.
What are the Risk Factors?
While anyone can get IC, it tends to strike under certain conditions:
- Elderly patients: Especially those with other health issues like heart disease, heart failure, high cholesterol or diabetes.
- Critically ill or hospitalized patients: Especially those with low blood pressure or sepsis.
- Younger individuals under physical or surgical stress: Such as during major trauma, cardiac surgery or previous abdominal surgery [1], [3].
Interestingly, one large study found that people under 80, men, those with abdominal tenderness and those who didn’t have visible bleeding were more likely to develop severe forms of the disease due to various risk factors [10].
Diagnosis of Ischemic Colitis
IC can be tricky to diagnose—especially in ICU settings where patients are already dealing with multiple issues. That’s why doctors take a multi-step approach for the diagnosis of ischemic colitis:
- Imaging Tests: A CT scan is often the first tool to show wall thickening or pneumatosis (gas in the wall of the colon). It may reveal thickening of the descending colon and proximal sigmoid colon, which are key for diagnosis and management.
- Lab Work: White blood cell counts, lactate levels and signs of infection may offer clues.
- Endoscopy: A colonoscopy or flexible sigmoidoscopy helps confirm the diagnosis and check how much of the colon is affected.
Diagnostic tests are essential to identify the condition accurately, allowing for proper treatment.
Since IC can mimic infections like C. difficile colitis or inflammatory bowel disease, ruling those out is a key step [5].
How is it treated?
Treatment depends on how bad the situation is.
Mild Cases:
- Bowel rest (nothing by mouth)
- IV fluids to maintain hydration
- IV fluids are critical for patient resuscitation, ensuring adequate organ perfusion during treatment
- Monitoring and supportive care
- Most patients recover within days without surgery. Acute ischemic colitis often resolves with medical care, which is key to reducing morbidity and mortality rates.
Severe Cases:
- Surgery is necessary when the colon has died (gangrene), there’s a perforation or peritonitis (infection of the abdominal cavity) sets in [9].Timing is everything here. Acting early—especially in severe cases—can be the difference between full recovery and life-threatening complications. Addressing the underlying cause of the low-flow state, if applicable.
Surgical Intervention
In severe ischemic colitis with dead tissue due to severely reduced blood flow, surgery may be needed. The main goal is to remove dead tissue, restore blood flow, and prevent complications, often involving colon resection. A colostomy might be necessary for healing. Surgical intervention depends on the severity, tissue damage, and patient health, aiming to prevent infection, remove dead tissue, and restore bowel function to improve prognosis [7].
Outcome
Ischemic colitis prognosis varies with severity and treatment timeliness. Mild cases often recover fully with supportive care (IV fluids, bowel rest, antibiotics). Severe cases have high mortality and may require surgery [11]. Prompt care generally leads to a good prognosis, but delayed intervention increases risks of tissue death, infection, and obstruction. Early diagnosis and treatment are crucial.
Closing Thoughts
Ischemic colitis isn’t a one size fits all disease. It’s better thought of as a spectrum of disorders with different causes, presentations and outcomes, including colonic ischemia and intestinal ischemia. In some cases it’s a passing event that resolves on its own. In others it’s a critical emergency requiring surgery.The challenge is it often goes undiagnosed especially in older or critically ill patients. Identifying any underlying condition that may be contributing to ischemic colitis is key to diagnosis and treatment. That’s why research and education around ischemic colitis is so important. By improving early detection and treatment, we can better manage this underdiagnosed but significant disease.
References
[1] Mosińska, P., & Fichna, J. (2015). Ischemic colitis: current diagnosis and treatment. Current drug targets, 16(3), 209–218. https://doi.org/10.2174/1389450116666150113120549
[2] Green, B. T., & Tendler, D. A. (2005). Ischemic colitis: a clinical review. Southern medical journal, 98(2), 217–222. https://doi.org/10.1097/01.SMJ.0000145399.35851.10
[3] Gandhi, S. K., Hanson, M. M., Vernava, A. M., Kaminski, D. L., & Longo, W. E. (1996). Ischemic colitis. Diseases of the colon and rectum, 39(1), 88–100. https://doi.org/10.1007/BF02048275
[4] Theodoropoulou, A., & Koutroubakis, I. E. (2008). Ischemic colitis: clinical practice in diagnosis and treatment. World journal of gastroenterology, 14(48), 7302–7308. https://doi.org/10.3748/wjg.14.7302
[5] Doulberis, M., Panagopoulos, P., Scherz, S., Dellaporta, E., & Kouklakis, G. (2016). Update on ischemic colitis: from etiopathology to treatment including patients of intensive care unit. Scandinavian journal of gastroenterology, 51(8), 893–902. https://doi.org/10.3109/00365521.2016.1162325
[6] Moszkowicz, D., Mariani, A., Trésallet, C., & Menegaux, F. (2013). Ischemic colitis: the ABCs of diagnosis and surgical management. Journal of visceral surgery, 150(1), 19–28. https://doi.org/10.1016/j.jviscsurg.2013.01.002
[7] Nikolic, A. L., & Keck, J. O. (2018). Ischaemic colitis: uncertainty in diagnosis, pathophysiology and management. ANZ journal of surgery, 88(4), 278–283. https://doi.org/10.1111/ans.14237
[8] Dimitrijević, I., Micev, M., Saranović, D.j, Marković, V., Petrović, J., Antić, S., Sekulić, A., & Krivokapić, Z. (2008). Ischaemic colitis--review. Acta chirurgica Iugoslavica, 55(3), 89–95. https://doi.org/10.2298/aci0803089d
[9] Sun, M. Y., & Maykel, J. A. (2007). Ischemic colitis. Clinics in colon and rectal surgery, 20(1), 5–12. https://doi.org/10.1055/s-2007-970194
[10] Hung, A., Calderbank, T., Samaan, M. A., Plumb, A. A., & Webster, G. (2019). Ischaemic colitis: practical challenges and evidence-based recommendations for management. Frontline gastroenterology, 12(1), 44–52. https://doi.org/10.1136/flgastro-2019-101204
[11] Huguier, M., Barrier, A., Boelle, P. Y., Houry, S., & Lacaine, F. (2006). Ischemic colitis. American journal of surgery, 192(5), 679–684. https://doi.org/10.1016/j.amjsurg.2005.09.018












